Measles
There has been a recent rise in measles cases in the UK (May 2023). Measles is spread when an infected person coughs or sneezes. It can spread very easily.
You can protect your child by making sure they get 2 doses of the MMR vaccine. Normally the 1st is given at 12 months and the 2nd around 3 years 5 months old. Even if you or your children have missed these vaccines, it’s not too late to get them. Contact your GP practice today.
If your child has had both doses of their MMR vaccine, there is almost no chance of them getting measles (unless they have a severely weakened immune system).
There is more information about the MMR vaccine and other childhood vaccinations.
What are the symptoms of measles?
Measles starts with:
-
fever
-
red, sore, watery eyes (conjunctivitis)
-
runny nose
-
cough

After a few days:
-
Small white spots may appear inside their mouth and on the back of their lips
-
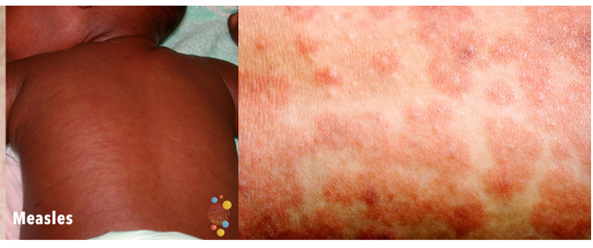
A rash. The rash starts on the face and behind the ears. It then spreads all over the body. The spots of the measles rash are sometimes raised and often join together to form blotchy patches. They are not usually itchy. The rash looks brown or red on white skin. It may be more difficult to see on brown or black skin
When should you worry?
If your child has any of the following:
-
Breathing very fast, too breathless to talk, eat or drink
-
Working hard to breathe, drawing in of the muscles below the ribs, or noisy breathing (grunting)
-
Breathing that stops or pauses
-
Is pale, blue, mottled or feels unusually cold to touch
-
Difficult to wake up, very sleepy or confused
-
Weak, high-pitched cry or can’t be settled
-
Has a fit (seizure)
-
Has a rash that does not go away with pressure (the ‘Glass Test’)
-
Is under 3 months old with temperature more than 38°C or under 36°C (unless fever in the 48 hours following vaccinations and no other red features)
You need urgent help
Go to the nearest Hospital Emergency (A&E) Department or phone 999
If your child has any of the following:
-
Breathing a bit faster than normal or working a bit harder to breathe
-
Dry skin, lips or tongue
-
Not had a wee or wet nappy in last 8 hours
-
Poor feeding in babies (less than half of their usual amount)
-
Irritable (Unable to settle them with toys, TV, food or hugs even after their fever has come down)
-
Is 3-6 months old with temperature 39°C or above (unless fever in the 48 hours following vaccinations and no other red or amber features)
-
Temperature of 38°C or above for more than 5 days or shivering with fever (rigors)
-
Temperature less than 36°C in those over 3 months
-
Getting worse or you are worried about them
If you are pregnant and haven't received 2 doses of the MMR vaccine, or if there are any children in your family who are under 12 months old or any child who hasn't had 2 doses of the MMR vaccine, please inform your GP practice urgently. They might need immediate treatment to protect them from getting measles.
If your child with measles has been in contact with someone who has a very weak immune system, let that person know about your child's measles. Ask them to contact their GP practice or NHS 111 urgently.
You need to contact a doctor or nurse today
Please call your GP surgery or contact NHS 111 - Go to 111.nhs.uk or call 111.(111 online does not currently take questions about children aged under 5, so if your child is 4 or younger, please call 111).
If symptoms persist for 4 hours or more and you have not been able to speak to either a member of staff from your GP practice or to NHS 111 staff, recheck that your child has not developed any red features.
If none of the above features are present:
-
Watch them closely for any change and look out for any red or amber symptoms
-
If your child has any other symptoms associated with their fever, you may want to look at the information on sore throat, cough, earache, diarrhoea and vomiting or tummy ache or our other pathways
-
Additional advice is also available to young families for coping with crying of well babies
-
If your child has a long term condition or disability and you are worried please contact your regular team or follow any plans that they have given you
Self care
Continue providing your child’s care at home. If you are still concerned about your child, call NHS 111 – dial 111
What should you do?
-
If you think your child has measles, let your GP practice know
-
Measles usually starts to get better in about a week
- To make your child more comfortable, you may want to lower their temperature using paracetamol (calpol) and or ibuprofen. If you've given your child ibuprofen and if they're still uncomfortable 2 hours later, you could try giving them paracetamol as well. If this works, you can alternate paracetamol and ibuprofen (every 2-3 hours), giving only 1 medicine at a time. Do not give more than the maximum daily dose of either medicine and more information on medicines can be found here
-
However, remember that fever is a normal response that may help the body to fight infection. Paracetamol and ibuprofen will not get rid of it entirely. Paracetamol and ibuprofen bring down the temperature but do not treat the infection. Whilst your child is unwell they will continue to get temperatures once the effects of the medicine has worn off
-
Avoid sponging your child. It doesn’t actually reduce your child’s temperature and may make your child shiver
-
Encourage your child to drink lots of fluids
-
If there are any crusts on your child's eyes, gently clean them using cotton wool soaked in warm water
-
Your child can spread the infection to others from the time their symptoms start until about 4 days after the rash appears
-
Children cannot go back to school or nursery until 4 days after the rash has started. They should also avoid contact with babies, pregnant women, people who have not had 2 doses of the MMR vaccine and people with weak immune systems
-
Finally, make sure that you and your partner are up to date with your MMR vaccines before getting pregnant. Measles can be extremely severe during pregnancy and can harm your unborn baby
Where should you seek help?
-
Unless your child has red features (see above), try to stay away from public places including pharmacists, GP practices and A&E departments as your child may spread their infection to others
-
If your child has any of the above amber features (see above), urgently contact your GP or call NHS 111. Make sure you let them know if your child has not been vaccinated against measles (MMR vaccine)
-
You should only call 999 or go to your nearest A&E department in critical or life threatening situations. Let a member of staff know as soon as you arrive if your child has not been vaccinated against measles (MMR vaccine)
What are the possible complications of measles infection?
Even in developed countries such as the UK, around one in every 15 children with measles will develop more serious complications. These can include:
-
ear infection (otitis media) in about 1 in 12 children with measles
-
pneumonia (chest infection) in about 1 in 16 children with measles
-
diarrhoea in about 1 in 12 children with measles
-
encephalitis (inflammation of the brain): 1 case for every 1000-2000 children with measles. Encephalitis can lead to permanent brain damage
-
measles causes death in about 1 in 5000 children with measles
In rare cases, measles can lead to a condition called SSPE (subacute sclerosing panencephalitis). This causes progressive destruction of the brain resulting in dementia, loss of motor function, fits (epilepsy), and eventually death. There is unfortunately no cure for SSPE.
Where should you seek help?
- If it is non-urgent, speak to your local pharmacist or health visitor
- If your child has any of the above features, urgently see your GP. For an urgent out-of-hours GP appointment, call NHS 111
- You should only call 999 or go to your nearest Emergency Department (A&E) in critical or life threatening situations
For wear and tear, minor trips and everything in between
Self-care
You can treat your child's very minor illnesses and injuries at home.
Some illnesses can be treated in your own home with support and advice from the services listed when required, using the recommended medicines and getting plenty of rest.
Sound advice
Children can recover from illness quickly but also can become more poorly quickly; it is important to seek further advice if a child's condition gets worse.
For information on common childhood illnesses go to What is wrong with my child?
Pharmacists are experts in many aspects of healthcare and can offer advice on a wide range of long-term conditions and common illnesses such as coughs, colds and stomach upsets. You don’t need an appointment and many have private consultation areas, so they are a good first port of call. Your pharmacist will say if you need further medical attention.
Sound advice
- Visit a pharmacy if your child is ill, but does not need to see a GP
- Remember that if your child's condition gets worse, you should seek further medical advice immediately
- Help your child to understand - watch this video with them about going to the pharmacy
For information on common childhood illnesses go to What is wrong with my child?
The 0-19 Service for children and young people is delivered by Oxford Health NHS Foundation Trust and offers a single point of access for Health Visiting, School Nursing and the Family Nurse Partnership. You can contact the teams using the details below:
Single Point of Access (SPA): 01865 903 800
Email: cyp0-19@oxfordhealth.nhs.uk
Chat Health Parentline
Text us any time for confidential advice and support and you will have a response the next working day (Monday-Friday exluding Bank Holidays).
Parents and carers for children aged 0-4: Text 07312 263 081
Parents and carers of children aged 5-11: Text 07312 263 227
Young people aged 11-19 and their parents and carers: Text 07312 263 08
Health Visitors
Health visitors are registered nurses or midwives who have additional training in community public health nursing. They provide a universal service, targeted to individual needs for children aged 0-5 years. Learn more about the Oxfordshire Health Visiting Service here!
School and college Health Nurses
School Health Nurses are specialist public health nurses and have offices across Oxfordshire. They work very closely with Health Visitors to support school aged children. They are available for young people to access in secondary schools and colleges, and offer a service to children who are home educated. They work closely with children, young people and their families to support and promote health and wellbeing. Learn more about the Oxfordshire School and college Health Nursing Service here!
Family Nurse Partnership
The Family Nurse Partnership service supports parents who are aged 19 years or under at conception, or under 21 years if they have been in care. The Family Nurse works alongside younger parents in their home, offering health, wellbeing and development support and information from the early stages of pregnancy, usually up until your child is two. Learn more about the Family Nurse Partnership service here!
GPs assess, treat and manage a whole range of health problems. They also provide health education, give vaccinations and carry out simple surgical procedures. Your GP will arrange a referral to a hospital specialist should you need it.
Sound advice
You have a choice of service:
- Doctors or GPs can treat many illnesses that do not warrant a visit to A&E
- Help your child to understand – watch this video with them about visiting the GP or going to a walk in centre
For information on common childhood illnesses go to What is wrong with my child?
If you’re not sure which NHS service you need, you can call 111 or use 111 online.
Please note that 111 online is for people aged 5 and over. Call 111 if you need help for a child under 5.
An adviser will ask you questions to assess your symptoms and then give you the advice you need, or direct you straightaway to the best service for you in your area.
Sound advice
Use NHS 111 if you are unsure what to do next, have any questions about a condition or treatment or require information about local health services
For information on common childhood illnesses go to What is wrong with my child?
Emergency Departments (A&E) provide vital care for life-threatening emergencies, such as loss of consciousness, suspected heart attacks, breathing difficulties, or severe bleeding that cannot be stopped. If you’re not sure it’s an emergency, call 111 for advice.